Cruel Confinement: Abuse, Discrimination and Death Within Alabama's Prisons
An investigation by the Southern Poverty Law Center (SPLC) and Alabama Disabilities Advocacy Program (ADAP) has found that for many people incarcerated in Alabama’s state prisons, a sentence is more than a loss of freedom. Prisoners, including those with disabilities and serious physical and mental illnesses, are condemned to penitentiaries where systemic indifference, discrimination and dangerous – even life-threatening – conditions are the norm.
An investigation by the Southern Poverty Law Center (SPLC) and Alabama Disabilities Advocacy Program (ADAP) has found that for many people incarcerated in Alabama’s state prisons, a sentence is more than a loss of freedom. Prisoners, including those with disabilities and serious physical and mental illnesses, are condemned to penitentiaries where systemic indifference, discrimination and dangerous – even life-threatening – conditions are the norm.
The Alabama Department of Corrections (ADOC) is deliberately indifferent to the serious medical needs of the prisoners in its custody. Inspections of 15 Alabama prisons, interviews with well over 100 prisoners and a review of thousands of pages of medical records, depositions and media accounts – as well as the policies, contracts and reports of the department and two major contractors – lead to one inescapable conclusion: Alabama’s prisons violate federal law protecting people with disabilities and the U.S. Constitution’s ban on “cruel and unusual punishments.”
This disregard for the law endangers the health and lives of prisoners. The ADOC’s actions demonstrate a valuing of cost over human life. The following are just a few examples of the consequences:
-
A prisoner who had survived prostate cancer had a blood test indicating his cancer had probably returned, but no follow-up test was given until a year and a half later. By that time, the cancer had spread to his bones and was terminal. He died less than a year later, in February 2014.
-
A prisoner undergoing dialysis died after he was given an injection of a substance that sent him into cardiac arrest in January 2014. Although there was a cart stocked with emergency medical equipment in the dialysis unit, no one present knew how to use it to save the man’s life.
-
A prisoner who had undergone abdominal surgery died after complaining to the medical staff that he was bleeding from his rectum. Although the man had requested two new pairs of pants the day he died because he kept bleeding through his clothes, the medical staff offered him only an antacid.
-
A prisoner incarcerated eight years ago after being shot in the groin had been told at the time of the shooting that he would have a catheter and a colostomy bag for six months before having surgery to repair damage from the gunshot. Almost a decade later, he has not had the surgery. He is in constant pain, sometimes urinating blood. He endures frequent infections from the catheter, often requiring hospitalization.
-
Numerous prisoners have had toes, feet or portions of legs amputated as a result of poor diabetes care. Some diabetic prisoners have reported that they have not had their blood sugar measured in months.
Psychiatric medication is often stopped or changed without any discussion between the psychiatrist and the patient.
Numerous prisoners have been placed under “Do Not Resuscitate” or “Allow Natural Death” orders without their consent or even their knowledge.
Prisoners with disabilities face many forms of discrimination. People in wheelchairs can’t access critical areas of facilities. At Kilby Correctional Facility, a wheelchair-bound prisoner is housed in a dormitory that has no wheelchair-accessible exits to the outside. The prisoner had no assistance when the facility was evacuated twice in May 2014, once for a fire and again for a gas leak. He had to struggle against the flow of evacuating prisoners to go farther into the prison to use a wheelchair-accessible exit.
Prisoners wishing to receive medical care are expected to complete a written form to request it – a potential hurdle for those who are blind or have cognitive disabilities. Blind prisoners are routinely asked to sign documents that they cannot read. The SPLC and ADAP have learned of two blind prisoners who unknowingly signed “Do Not Resuscitate” orders.
The state’s legal responsibilities are clear: Alabama has a constitutional obligation to provide adequate medical and mental health care to individuals in its custody. In 2011, the U.S. Supreme Court found in Brown v. Plata that depriving prisoners of adequate medical care “is incompatible with the concept of human dignity and has no place in civilized society.” Deliberate indifference to these medical needs constitutes “unnecessary and wanton infliction of pain” barred by the Eighth Amendment.
Alabama also must ensure that its prisons, programs, activities and services are accessible to prisoners with disabilities under Title II of the Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973. Instead, the ADOC systematically violates federal law, leaving people with disabilities isolated, unable to participate in prison programs and deprived of the medical care they need.
Alabama illegally operates a corrections system that is little more than a network of human warehouses, a place where individuals caught in the criminal justice system are banished and forgotten.
A conviction does not open the door for the state to engage in cruelty. Whenever Alabama determines a person must be incarcerated, it must accept the legal – and moral – responsibility that comes from imprisoning a human being.
This report is the result of an investigation by the Southern Poverty Law Center (SPLC) and the Alabama Disabilities Advocacy Program (ADAP). It is based on inspections of Alabama’s 15 prisons; interviews with more than 100 prisoners; a review of thousands of pages of medical records as well as depositions and media accounts; and the policies, contracts and reports of the Alabama Department of Corrections (ADOC) and two of its major contractors. The principal writer was Maria Morris, managing attorney of the SPLC’s Montgomery Legal Office. Contributing writers were J. Patrick Hackney and William Van Der Pol Jr., both staff attorneys for ADAP. The report was edited by Jamie Kizzire and designed by Sunny Paulk, both of the SPLC. For further information, see the SPLC’s letter to the ADOC at http://sp.lc/LetterToCommissioner.
About the Southern Poverty Law Center
The Southern Poverty Law Center is a Montgomery, Alabama-based nonprofit organization dedicated to fighting hate and bigotry and to seeking justice for the most vulnerable members of our society. Using litigation, education and other forms of advocacy, the SPLC works toward the day when the ideals of equal justice and equal opportunity will be a reality.
About the Alabama Disabilities Advocacy Program
The Alabama Disabilities Advocacy Program (ADAP) is part of the nationwide federally mandated protection and advocacy (P&A) system. ADAP’s mission is to provide quality, legally-based advocacy services to Alabamians with disabilities in order to protect, promote and expand their rights. ADAP’s vision is one of a society where persons with disabilities are valued and exercise self-determination through meaningful choices, and have equality of opportunity.
The Alabama Department of Corrections had 25,055 prisoners in in-house custody as of March 2014. This means the department is responsible for the health and well-being of a population comparable to the Birmingham suburb of Homewood (population: 25,262, according to 2012 U.S. Census estimates).
Yet there are only 15.2 doctors and 12.4 dentists for this city behind bars.1 A doctor’s average caseload is 1,648 patients and a dentist’s is more than 2,000 patients.
Overall, Corizon Inc., which has the contract to deliver medical services to these prisoners, provides a medical staff of 493 people (including doctors, nurses, administrative and records staff). The ratio of total medical staff to prisoners is 1:51. Even at the Kilby Correctional Facility in Mt. Meigs, which is home to the ADOC hospital and is where all prisoners go through an intake assessment, doctors are scarce. There is just one full-time and one half-time doctor on staff for more than 2,000 prisoners.
This extraordinary understaffing has led to a multitude of problems. The vast majority are easily predictable: delays, failures to diagnose and treat problems, failure to follow up with patients, errors and decisions to not treat seriously ill prisoners. There should be no doubt that this understaffing is a direct result of the ADOC’s bid process for its medical services contract, a process that placed far greater emphasis on cost than any other factor.
Numerous prisoners have complained of symptoms for months without anyone addressing their concerns, only to be diagnosed with advanced stage cancer that is terminal by the time it is diagnosed. In mid-2011, a prisoner who had been treated for prostate cancer in 2006 began showing a dramatic rise in the levels of a protein that is the main indicator of prostate cancer – a sign his cancer had returned. He began vomiting frequently, sometimes even throwing up blood. He was not given necessary tests or diagnosed until a year and a half later: February 2013. By that time, his prostate cancer had spread to his bones. He died in January 2014.
A prisoner incarcerated eight years ago after being shot in the groin had been told at the time of the shooting that he would have the catheter and colostomy bag for six months before having surgery to repair damage from the gunshot. Almost a decade later, he has not had the surgery. He is in constant pain, sometimes urinating blood. He endures frequent infections from the catheter that often require hospitalization.
Prisoners have lost toes, feet or portions of legs as a result of poor diabetes care. One diabetic prisoner had a toe amputated in February 2013 after a blister on it went untreated for six weeks, despite his repeated requests for medical assistance. After his toe was amputated, he did not receive proper care at the Kilby Correctional Facility infirmary. His surgical wound became infected, resulting in a second toe being amputated in July 2013.
Another diabetic prisoner estimates that in the two years he has been in the ADOC’s custody, he has passed out 15 to 20 times from having low blood sugar. In the fall of 2013, a new doctor arrived at Kilby and changed the medications of many of the diabetics without examining them. Some diabetic prisoners have reported that they have not had their blood sugar measured in months.
A September 2012 report from Corizon states that there were 2,144 prisoners with hepatitis C but only four of them were receiving treatment. A prisoner at Holman Correctional Facility in Atmore recently died from complications from hepatitis C after going without treatment. Another prisoner at Holman Correctional Facility reports that he watched several men with hepatitis C become jaundiced as their disease progressed without treatment and their livers begin to fail.
Staph infections also are rampant. Numerous prisoners end up being sent to the hospital as their untreated infections progress and become septic or develop into cellulitis – both serious complications. One prisoner reported that he had a staph infection on his leg, which became swollen. Yet, he was not approved to have intravenous antibiotics and was not treated. After his leg turned black, he underwent emergency surgery to remove the infected area. Another prisoner estimates six men in his dormitory at St. Clair Correctional Facility had staph infections in April 2014. A prisoner at Bibb Correctional Facility sleeps in a bunk next to a man with a hole the size of a quarter in his cheek that oozes pus and blood.
Slow or nonexistent emergency response
Even prisoners with broken bones, burns or other emergency conditions have waited hours, days or months for treatment, the SPLC and ADAP found. A prisoner who had undergone abdominal surgery died after complaining to the medical staff that he was bleeding from his rectum. Although the man had to ask for two new pairs of pants on the day he died because he kept bleeding through his clothes, the medical staff offered him only an antacid.
At Elmore Correctional Facility, a prisoner had an adverse reaction to some substance on May 16, 2014. He was taken to the infirmary, where he writhed around, repeatedly falling off his bed. He was not given any treatment. Three days later, he was finally taken to the hospital where he died.
At St. Clair Correctional Facility, nurses in November 2012 told a doctor that a dialysis patient was in pain following his treatment. The doctor instructed the nurses to give the man some water and return him to his dorm. He also told the nurses they should not call him again or send the man to the hospital. The prisoner returned to the infirmary several times during the night, but each time was sent back to his dorm. He died in the early hours of the morning.
A prisoner with a broken foot was not treated for nine months, at which point the bones had begun to heal incorrectly. Another prisoner with a broken kneecap waited nearly two months for medical care. By the time he was treated, the kneecap could no longer be fixed. A prisoner who complained of a sore, swollen testicle was given only ice for five days. It was then determined that he had gangrene: His testicle had to be removed.
Even prisoners who have suffered strokes say there was a delay in treatment. One man lay on the floor of his cell for four days before medical staff saw him following a stroke. He was left partially paralyzed on one side of his body. Another prisoner had a stroke one evening while at a work release center. He was sent to the hospital unit at the Kilby Correctional Facility rather than a local hospital. There was no doctor on duty at Kilby, and the medical staff waited until the doctor came in the following morning to send the prisoner to the hospital. This meant the prisoner was not treated for his stroke until more than 12 hours after it occurred. He is now confined to a wheelchair.
A prisoner at Kilby was forced to wait seven hours to be taken to the hospital after grill cleaner splashed in his eyes. A prisoner at Holman who had a flaming cloth thrown on him in his cell by other prisoners was not taken to the hospital until more than a day later.
Failure to manage outbreaks
The ADOC also has no effective system for preventing or managing infectious diseases. The U.S. Supreme Court has repeatedly recognized that exposing prisoners to infectious diseases can constitute a violation of the Eighth Amendment.2
Recent years have seen numerous tuberculosis (TB) outbreaks in Alabama’s prisons. In the fall of 2013, a guard at Tutwiler Prison for Women had active TB but was allowed to continue working – even after officials were aware of the guard’s condition. The staff was eventually tested for TB, but many prisoners where the guard was stationed have not been tested.
SPLC investigators have both witnessed and heard that the dorms where prisoners are found to have TB are not effectively quarantined. In the summer of 2012, the SPLC and ADAP visited Donaldson. The warden stated that one of the dormitories was under quarantine for TB. The SPLC and ADAP were permitted to enter, and prisoners were wandering in and out of the dorm and mixing with prisoners from other dorms. At St. Clair, in January and February 2014, several men were diagnosed with active TB. One worked in the kitchen until the day he was diagnosed. Another prisoner at St. Clair reported that during his last physical in the summer of 2013, neither he nor the group of the 60 to 70 prisoners going through the physical process with him were given TB tests.
There was also a recent outbreak of scabies, a contagious skin disease, at the Tutwiler, St. Clair and Ventress correctional facilities. Prisoners report that, contrary to the statements made by the ADOC in the media about the outbreak at Ventress, there has been a scabies infestation there for years. In response to this outbreak, prisoners were instructed to place their mattresses over a fence in the yard during the day to air them out. When they collected the mattresses at night, there was no way to ensure that each person received the same mattress. The U.S. Supreme Court has recognized the mingling of mattresses where prisoners had infectious diseases as a constitutional violation.
The conditions within the state’s prisons, which are grossly overcrowded, make spread of disease nearly inevitable. Prisoners in every facility report the presence of vermin, especially rats and spiders. At the Fountain Correctional Facility in Atmore, there were large amounts of what appeared to be rat droppings on cans of food in the kitchen. At Holman, the SPLC was informed that a bird had been flying around in the kitchen for several weeks. What appeared to be bird droppings were found on a bed in a prison dorm.
Prisoners at several facilities have reported problems with the plumbing. They describe repeated sewage overflows, including incidents at Ventress Correctional Facility where prisoners were required to carry raw sewage away to be dumped on the edges of the prison grounds. At the Hamilton Aged and Infirmed Center, there is a footbridge across a canal of raw sewage.
It is clear from physical inspections of Alabama’s prisons that the showers, toilets, sinks and other physical infrastructure cannot withstand the challenges of housing twice as many people as the prisons were intended to hold. Such conditions violate the Eighth Amendment.4 This failure is not only evident in the stories told by prisoners but by the very uniforms they must wear. The uniforms, like their bedding, are unclean because the laundry facilities simply cannot produce water hot enough to adequately clean them.
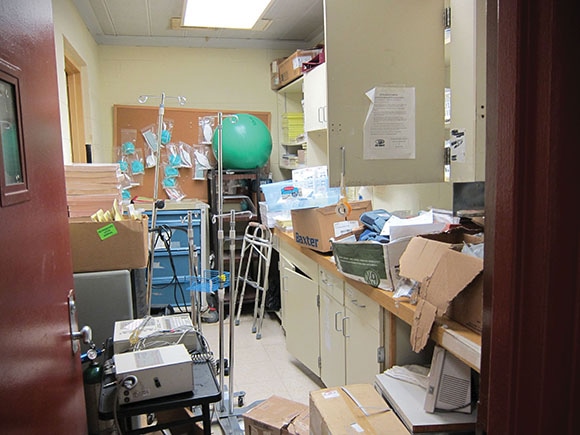
Medication errors
Several prisoners in various prisons recounted stories to the SPLC and ADAP of people who died after receiving the wrong medication. One prisoner received an injection as he underwent a dialysis treatment in January 2014. After the substance, which is still unknown to the SPLC and ADAP, entered the prisoner’s bloodstream, he went into cardiac arrest. The prison’s dialysis unit included a cart stocked with emergency medical equipment. But no one present that day knew how to use the equipment. The prisoner died.
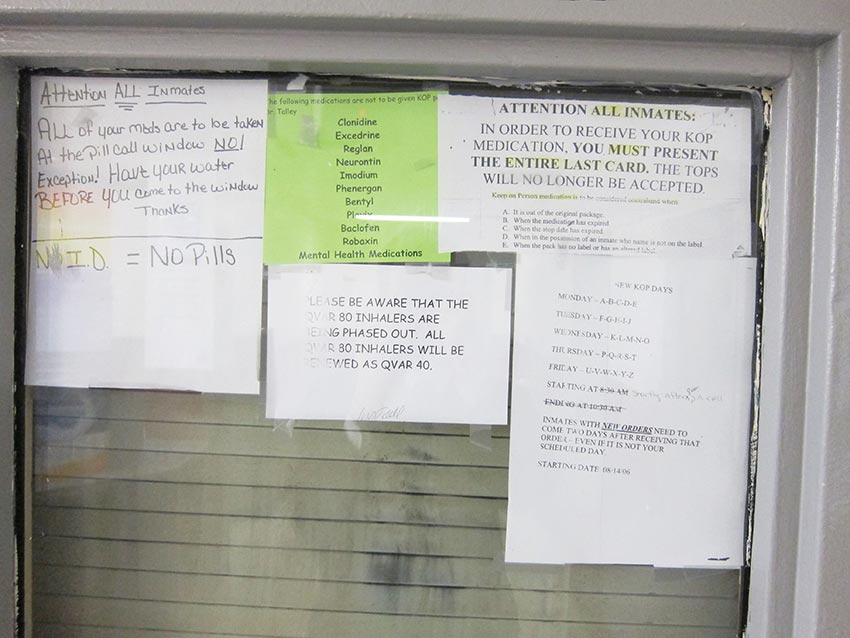
Many prisoners are given the wrong medicine. One prisoner recalled five instances of receiving the wrong medication. Another was given the wrong medicine and was left unable to walk or talk for about 10 hours. Nearly all prisoners interviewed reported that they were not informed of the purpose, side effects and benefits of the medications prescribed to them.
Numerous prisoners have reported that they have had problems receiving medication within the prison system. A prisoner prescribed a medication for mental health symptoms along with a second medication to control its side effects reported that she is routinely denied the medication for the side effects. Other prisoners report that medications they had been taking for years have been abruptly discontinued even though they had not seen their doctors.
At Bullock Correctional Facility, a prisoner with a seizure disorder found his seizure medication discontinued because he slept through his 4 a.m. pill call a few times. He slept through pill call because his mental health medications make it difficult for him to wake up. He has had two seizures since being taken off the medication.
Interference and indifference
Another obstacle for prisoners seeking medical help is the corrections officers. The SPLC and ADAP found many instances where officers delayed or denied access to medical care. At St. Clair Correctional Facility a prisoner in segregation suffering from abdominal pain and constipation asked for help only to have correctional officers refuse to take him to the infirmary. Over a period of weeks, the correctional officers told him the pain was only acid reflux. The prisoner was eventually taken to a hospital for emergency surgery on a severe bowel obstruction.
At Fountain Correctional Facility in March 2013, correctional officers refused to let a prisoner with a large infected wound go to the infirmary, although he had instructions to return to the infirmary every day to have the dressing on the wound changed. As result, the infection became worse.
In December 2013 at Holman Correctional Facility, a prisoner on suicide watch had a flaming cloth thrown on him by other prisoners, causing burns on his legs. The guards put the fire out, but refused to take him to see medical, saying the burns were “nothing.” It was not until more than 24 hours after the assault that the man was sent to medical and then the hospital.
Prisoners also say when they receive medical treatment, corrections officers are present. The officers sometimes tell the medical staff treating the prisoner that the prisoner is lying, or at least suggest that the patient isn’t being truthful.
One prisoner in segregation at St. Clair passed out five different times in May 2014. Each incident occurred late in the day, several hours after the prisoners are fed their dinner. There were no guards in the unit. Each time this prisoner passed out, it wasn’t until the guards made their rounds the next morning that they discovered he had passed out.
Prisoners with disabilities face obstacles to health care
Numerous prisoners have expressed concerns over Corizon or the ADOC failing to provide medical supplies, equipment and personal assistance. One prisoner who contacted the SPLC and ADAP stated that the ADOC lost his prosthetic leg and refused to replace it. Where prisoners with disabilities are able to get assistance from other prisoners, they have to pay for the assistance with tasks such as going to the cafeteria, completing medical call slips, going to pill call and bathing.
Even those who are able to pay are not always able to get assistance. A wheelchair-bound prisoner at Kilby, who is paralyzed on one side, has tried to get people to help him, only to have the guards say that it is not permitted. He often misses pill call because, without assistance, it is very difficult for him to get to the pill call window.
Prisoners with vision or hearing impairments also encounter numerous obstacles in accessing medical care. There is no mechanism for assisting prisoners who cannot see to fill out sick call slips. There also are no sign language interpreters to assist prisoners who cannot hear. Frequently, medical personnel have individuals who cannot see well enough to read their documents sign forms without explaining what they are about.
The SPLC and ADAP have spoken with two prisoners who are blind and unknowingly signed “Do Not Resuscitate” orders. In one case, the prisoner learned of the Do Not Resuscitate order when the ADOC cited it as the reason the prisoner could not have the cataract surgery he needed.
The ADOC’s contractual agreement with Corizon and MHM Correctional Services, the mental health services contractor, does not include provisions to ensure effective communication with patients with impaired hearing or vision. Neither contractor appears to have any policies or staff to address such needs.
More than 3,000 prisoners in Alabama prisons were receiving some form of mental health treatment in March 2013, according to an ADOC mental health report. This population was distributed throughout the prison system’s facilities. Other than the Hamilton Aged and Infirmed Center, every medium or maximum security facility housed at least 100 prisoners on the mental health caseload.
Despite the fact that every facility housed a significant number of individuals taking psychiatric medication, the level and quality of staffing at Alabama Department of Corrections facilities is woefully inadequate. There are just 4.7 full-time psychiatrists in the facilities. At many prisons, there is no psychiatrist.
The level of staffing is clearly insufficient. Several prisoners report that, despite being prescribed psychiatric medications, they do not receive periodic check-ups with a psychiatrist. Often, the only contact they have with any mental health professional is when they are acutely mentally ill and exhibiting suicidal ideations or actions.
There are only 5.6 psychologists for the entire system. Only Tutwiler Prison for Women has a full-time psychologist on staff. Psychologists work at just six facilities: Donaldson, Bullock, Limestone, Holman, Kilby and Tutwiler. At all other facilities, no psychologist is available.
This failure by the state to adequately staff its facilities is even more astonishing when viewed from a historical perspective. In the 1970s, when Alabama prisons were about one-sixth as large as they are now, the level of mental health staffing was found to be unconstitutionally low.5 There was one full-time psychologist in the system at that time. Remarkably, the current ratio of psychologists to prisoners is roughly half of what it was then.
Even the ADOC does not believe the current mental health staffing levels are adequate. When the ADOC issued a recent request for mental health services contract proposals, it cited the minimum staffing need to be 144.95 full-time employees. Under the current contract, MHM, the mental health services contractor, is not providing even this number of mental health staff. The new MHM contract provides for just 126.5 full-time employees.
Failure to identify mentally ill prisoners
Only 12.2 percent of the prison population is identified as having any mental health issue. This almost certainly indicates that Alabama is not identifying prisoners with mental health disorders. A 2006 Department of Justice study of prison and jail prisoners throughout the country found that about half of the prisoners in state correctional facilities meet the criteria for a mental illness found in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). It is highly unlikely that Alabama’s prisoners suffer from mental illness at just one-quarter of the rate of most state prison populations. The failure to identify prisoners in need of mental health care or to provide them with the level of care needed is a violation of the Eighth Amendment.
It is evident from the joint SPLC and ADAP investigation that the ADOC under-identifies prisoners with mental health disorders.
One prisoner at St. Clair cut himself with razor blades on five separate occasions, but never received mental health care despite his numerous requests. Instead, corrections officers mostly expressed their frustration with the prisoner, even beating him on one occasion. When the prisoner cut himself so severely that he cut a tendon in his forearm, a corrections officer asked him why he insisted on mutilating himself on his shift.
“Why don’t you just go ahead and kill yourself?” he asked the prisoner.
Shortly thereafter, a nurse came by and the prisoner showed the nurse his arm. The nurse said he would return when he had time, but did not come back. The prisoner was taken out of his cell and placed in a cell outside. He was beaten by two officers in the cell and left there for another hour before he was taken to the infirmary.
The nurse at the infirmary attempted to staunch the blood flow from his arm, but was unable to do so. An hour later, he was taken to Brookwood Medical Center in Birmingham, where several staples were put into his arm to hold the wound closed – approximately five hours after he mutilated his forearm.
One prisoner reported hearing voices and engaging in self-harm thousands of times over a period of about eight years before finally being identified as needing mental health care. Another prisoner was placed on suicide watch three times within four months and asked for mental health treatment, but has not been given any treatment. A prisoner who repeatedly mutilated himself was threatened with forced medication by staff. Just two weeks later, he asked to be placed on the mental health caseload only to have the request refused.
There is also evidence that the ADOC is dramatically under-identifying the level of acuity of those who are mentally ill.
According to ADOC mental health codes, MH-1 and MH-2 are used for prisoners with “mild impairment in mental functioning, such as depressed mood or insomnia.” MH-3 is for moderate impairments “such as difficulty in social situations and/or poor behavior control.” MH-4 is for severe impairments “such as suicidal ideation and/or poor reality testing.” MH-5 is used for severe impairments “such as delusions, hallucinations, or inability to function in most areas of daily living.” MH-6 – the code for the most acutely mentally ill – is reserved for prisoners who have been committed to a mental hospital.
As of March 2013, just 234 prisoners in ADOC custody – less than 1 percent – were classified at greater than MH-2. In contrast, the Department of Justice study cited above found that, nationally, some 43 percent of state prisoners met the DSM-IV criteria for mania and 15 percent met the criteria for psychotic disorders. It is extremely likely that far more of ADOC’s prisoners should have a higher mental health code.
The SPLC and ADAP have spoken with a number of prisoners who report hallucinations but are either not on the mental health caseload at all or are classified as either MH-1 or MH-2. The SPLC and ADAP have heard of numerous severely mentally ill prisoners who are housed in general population where they are victimized by other prisoners and, in some cases, are dangerous to other prisoners as well as to themselves. The SPLC and ADAP have met with mentally ill prisoners unable to carry on even the most basic coherent conversation. These prisoners are, in some instances, at facilities that house no one with a mental health code higher than MH-2.
Even the ADOC’s own documents show the acuity of prisoners’ mental illness is understated. According to the March 2013 report, only 222 people were categorized as MH-3, and just 12 people were classified at higher mental health codes. Yet, 853 people were, at that time, diagnosed with psychotic disorders – disorders that would clearly, per the ADOC description of mental health classifications, classify a person as MH-5.
Medication denied
The ADOC barely spends $1 per patient, per day on psychiatric medication. Even more astounding is that the ADOC’s annual expenditure for psychiatric medication actually decreased by 26 percent from March 2010 through March 2012, despite the relative stability of the state’s prison population.
The investigation by the SPLC and ADAP uncovered instances of mentally ill prisoners being denied access to necessary psychiatric medication as well as issues with medication management. These failures by the ADOC to provide, prescribe and manage necessary psychiatric medications to its prisoners violate the Eighth Amendment.
There are numerous, credible reports that psychiatric medication is improperly decreased, ended or changed to less effective forms. Some prisoners report being on psychiatric medications for years and then being taken off their medications – and the mental health caseload – despite needing treatment. This includes prisoners exhibiting suicidal thoughts and actions. Even after numerous suicide attempts, prisoners’ medications are not reinstated nor are they returned to the mental health caseload.
Prisoners entering the prison system or transferred within it often face lengthy periods where they are denied psychiatric medications and are not properly monitored until seen by the staff at the new facility. The SPLC and ADAP found numerous instances of medication being denied to prisoners when they are transferred into a new facility. There is also little or no follow-up to ensure the efficacy of the medication. The lack of staff experienced in monitoring the medication ensures that it is practically impossible for necessary monitoring to occur.
The SPLC and ADAP have received numerous reports from prisoners who have never received any form of regular, face-to-face consultations with a psychiatrist despite being on the mental health caseload for years. Many report that the only time that they have ever had a face-to-face consultation with a psychiatrist is during an acute mental health crisis. In most instances, this contact is limited to someone with less experience than a psychiatrist, such as a nurse practitioner or a mental health counselor.
When prisoners receive psychiatric medication that increases their heat sensitivity, care must be taken because they are more prone to heat stroke and heat-related illnesses. Other than the residential treatment units, none of the ADOC facilities that routinely house prisoners on psychiatric medications have air conditioning. And as of May 2014, the air conditioning in three of the seven dormitories in Bullock’s residential treatment unit is not working.
The SPLC and ADAP found a prisoner on psychiatric medication that increases heat sensitivity in a dormitory where the air conditioning is not working. In May 2014, the prisoner endured temperatures in the 90s. This prisoner, who has difficulty carrying on a coherent conversation and does not read well, was asked by prison officials to sign a paper promising to tell the correctional officers if he was getting too hot.
Prisoners medicated against their will
Numerous prisoners report being forced to take medication under circumstances that do not comport with due process requirements. Two prisoners reported being forcibly medicated for years but had no recollection of any proceeding that determined that they could be medicated against their will.
When one of these prisoners told a nurse that he did not want to continue taking medication, he was threatened with segregation. Several prisoners report being sent to segregation until they agree to take the medication. One man was kept in segregation for 15 days for refusing his medication.
One prisoner was forcibly medicated even as he awaited a determination of whether he was seriously mentally ill and could be forced to take medications. In the end, it was determined that he was not seriously mentally ill and could not be medicated against his will. Prisoners at the Bullock Correctional Facility, which maintains a specialized unit for the most severely mentally ill known as the Intensive Stabilization Unit, have reported being forcibly medicated for talking back and other behavior that met with the staff’s disapproval. Prisoners reported that this occurs at other facilities as well.
Another prisoner reports that he refused his medication, Prolixin, because it made him shake – a well-known side effect. This resulted in an officer slapping him and wrestling him to the ground. The officers told him that they were going to put him in segregation for refusing his medication. He was able to explain to them that he needed to see the psychiatrist because he was suffering from the medication’s side effects. The officers offered a deal: If the prisoner took his medicine, they would tell the psychiatrist to see him. They also would not put him in segregation. The prisoner agreed, but it took 30 days for him to see the psychiatrist.
This prisoner has refused his medication on a number of occasions. When he refuses, officers tell him that he will be forcibly held down and given his medication. This prisoner has never had a hearing to determine whether he should be permitted to refuse his medication.
He has witnessed other prisoners refuse to take their medication as well. Sometimes they are held down and forced to take it. Other times, the threat of forced medication is enough to change their mind. They are even taken to segregation until they start taking the medication.
Seriously mentally ill in poorly equipped facilities
On paper, the Bullock Correctional Facility’s unit for severely mentally ill prisoners had plenty of space to care for such prisoners in early 2013. A March 2013 ADOC report showed seven people were housed in the Intensive Stabilization Unit, which was listed as having beds for 30 people. Only two people had been there for more than 30 days. The report painted a picture of a unit ready to accommodate prisoners with the most serious need for mental health care.
The reality was much different.
During an SPLC and ADAP inspection, the unit was full, which is almost always the case, according to ADOC staff at the inspection. Half the unit was used for segregation of individuals not on the mental health caseload. This means that if a prisoner became acutely mentally ill, there would not be a cell available in this unit unless someone is removed.
The SPLC and ADAP interviewed numerous prisoners who said when they become acutely psychotic and a danger to themselves, they are placed in a “suicide cell” because there’s no other place for them. Treatment for prisoners in suicide cells consists of mental health staff making a once-a-day pass where they ask – through the door – whether the person is still suicidal. The staff member usually spends less than five minutes with the patient. One prisoner said this pass often occurs in the early morning hours when prisoners are likely to be asleep.
One prisoner with a mental health code of MH-5 (severe impairment) was housed at Easterling Correctional Facility, which lacks any psychiatric staffing. Three prisoners with a mental health code of MH-3 (moderate impairment) were housed at ADOC facilities not designed to care for MH-3 prisoners.
Some mentally ill prisoners are housed for years on end in segregation units throughout ADOC facilities because of their acute mental illness. These prisoners are referred to as being “on the circuit” and are moved between the segregation units at Holman, Donaldson and St. Clair. One man, currently in segregation at Donaldson, has been on the circuit for five years. They receive little or no mental health care in the segregation units.
Even when prisoners are in a Residential Treatment Unit (RTU), they still may not receive the care they need. By the end of March 2013, there were 270 individuals in the RTUs. Yet there were only 243 individual contacts by psychiatrists with the RTU patients over the course of the month. There were 42 contacts with a psychologist and 76 contacts with a nurse practitioner. Prisoners report that these contacts last just minutes, often at the cell door or in settings that are not confidential and offer little therapeutic value.
Abuse by guards also appears to be much worse in the mental health units than elsewhere in the prison system. Numerous prisoners have reported an extraordinary level of violence and abuse by guards in the Bullock mental health units. They describe guards knocking over bunks if prisoners are not quick enough to get up in the morning, although many are under the influence of medications to help them sleep.
One prisoner in the mental health unit at Bullock describes having to clean up the blood of another prisoner who had been beaten by guards. In another incident, when a prisoner tried to change the television channel, the guard told him to get away from the TV set. He then spit in the prisoner’s face before beating him with a baton. After the beating, the prisoner was sent to the infirmary where his head was stitched up. The prisoner was then placed in segregation.
Years earlier, the same prisoner was beaten because he was loudly responding to auditory hallucinations. The guards became agitated and beat him, breaking his jaw and a rib. He was not taken to medical at all. He was placed in segregation. Six months later, X-rays revealed his broken bones.
Prisoners also report that guards often use pepper spray in the mental health units and on the mentally ill. Several prisoners described an incident where a guard used pepper spray on a prisoner after a fight, despite the fight being long over by the time the guard doused the prisoner. The guard held out his pepper spray can after the fight ended, causing the prisoner to put his hands in front of his face. The guard told him to put his hands down. He even went as far as telling the prisoner that he would spray him a second time if he put his hands in front of his face or closed his eyes. He then sprayed the prisoner, despite the fight being long over by that time. The mentally ill prisoner did not put his hands in front of his face.
A failure to protect
The ADOC also fails to protect prisoners in the most elementary way: Keeping razor blades out of the hands of suicidal prisoners. The department provides prisoners with disposable razors in their cells for shaving, but they are never collected or accounted for by prison authorities after use. This is true in Residential Treatment Units as well. Even individuals with a documented history of using a razor in recent suicide attempts are given razors.
Prisoners have the right “to receive medical treatment for illness and injuries, which encompasses a right to psychiatric and mental health care, and a right to be protected from self-inflicted injuries, including suicide.”6 The ADOC does protect prisoners from self-harm. The results are predictable and potentially lethal.
One individual, on two separate occasions in two separate facilities, used a razor to attempt suicide while in a suicide watch cell. He used the same razor blade he had used in the initial attempts in his cell and brought it with him to the suicide watch cell. The guards failed to appropriately search the prisoner before placing him in the suicide cell.
Another prisoner, who has a long history of self-mutilation with sharp objects, was housed in segregation at Fountain in March 2014. After intentionally cutting himself with a razor, he did not receive any mental health counseling. Instead, the episode marked the beginning of a series of incidents where the prisoner cut himself – even when he was confined to a suicide-watch cell. After one cutting incident in the suicide-watch cell, the guards failed to remove the razor, which the prisoner turned on himself once he was returned to it. The guards simply did not believe the prisoner when he reported there was a razor in his suicide-watch cell. Instead, the guards assumed the prisoner was cutting himself on a rusty air vent, which resulted in him getting a tetanus shot.
People with disabilities often encounter discrimination throughout the prison system. They are segregated from other prisoners. They are excluded from work release programs solely for their disabilities. Prisoners in wheelchairs can’t access parts of the prisons even when these barriers could be removed with relative ease and limited expense. A hearing-impaired prisoner reports being hit by a corrections officer for not responding to an order he couldn’t hear.
Quite simply, the ADOC systematically violates federal law, including Title II of the Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973, which prohibit discrimination against people with disabilities, including those in prisons.
Guards at some facilities have informed prisoners in wheelchairs that they cannot be pushed by other prisoners. Several of the prisoners who have reported this issue to the SPLC have had strokes and have limited use of one hand, making it nearly impossible to push their own wheelchairs. This policy excludes wheelchair-bound prisoners from the most basic services of the prison system, including medical care, food and even access to bathroom facilities.
When a prisoner needs medical care, he or she must complete a written form requesting it. Every ADOC facility has boxes to submit the medical slips. It may seem like a simple process, but for a prisoner with an intellectual disability or vision impairment, filling out a form can be a major obstacle.
Prisoners with disabilities also have reported that they are excluded from work release programs due solely to their disabilities. One prisoner was sent to a work release program, and then told that he could not participate because he is blind. The same thing happened to another prisoner who is deaf. Another prisoner has been excluded from work release solely because of his medical code, a code that is based not on any medical condition but on his disability. Work release is a critical benefit, allowing prisoners to develop skills, reintegrate into society, earn money and demonstrate parole readiness. A policy of excluding prisoners with disabilities clearly violates the Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973.
The ADOC also must provide auxiliary aids and services necessary for effective communication with prisoners with disabilities.7 These aids and services may include large print materials for prisoners with low vision or a sign language interpreter for prisoners with deafness. But prisoner accounts show that the ADOC has failed to provide them.
One deaf prisoner, who has been in the prison system for several years, has never been offered a sign language interpreter, though he requested one on numerous occasions. This prisoner states that he does not understand certain ADOC policies and cannot participate in any programs offered by the prison due to this inability to communicate.
To make matters worse, staffers often rely on other prisoners to “communicate” with the prisoner with deafness. On at least one occasion, the prisoner was denied a sign language interpreter for a disciplinary hearing. He did not understand the proceedings and was sentenced to a 30-day segregation term.
A prisoner who had two hearing aids because he is mostly deaf in both ears ended up with only one functioning hearing aid after personnel from the ADOC and Corizon, the medical services contractor, told him that he would only be provided with one. He now frequently loses his balance because he has only one functioning hearing aid. He often has to wait a long time for a replacement battery for it, during which he can hear very little. On one occasion, he was assaulted by a correctional officer for failing to obey an order that he could not hear.
Several other prisoners have also described incidents where they were verbally or physically mistreated due to their disabilities. At the Kilby Correctional Facility A Dorm, where prisoners who are blind or in wheelchairs are concentrated, guards have taunted prisoners about their disabilities. A blind prisoner reported that guards wave their hands in front of his face, refer to him as “blind man,” and make jokes about the “blind train” – the line formed when blind prisoners lead each other to the dining room or to pill call. A prisoner also reports that when prisoners in wheelchairs complain about an issue the guards respond by asking, “What are you going to do about it? You can’t get up.”
A blind prisoner also reported being assaulted by a guard during prisoner count. The prisoner sat up in bed as he usually does during the count when the guard yelled at a prisoner to stand up. The guard kept yelling, identifying the person only as “you.” The prisoner did not know that he was the person being told to stand up. The guard threw the blind prisoner to the floor for disobeying. He then wrote the prisoner up for disobedience. Disciplinary hearing records show the prisoner pleaded guilty at the hearing, but the prisoner says he did not plead guilty and no one even told him that the record indicates such a plea.
Architectural barriers
Under the Americans with Disabilities Act, the ADOC is generally not required to undertake architectural renovations to improve accessibility for facilities built before 1992, but it must remove architectural barriers when it can be done with relative ease and at limited expense. It also must ensure that it operates “each service, program, or activity so that the service, program, or activity, when viewed in its entirety, is readily accessible to and usable by [prisoners] with disabilities.” It is also discriminatory to deny a prisoner access to and participation in services, programs and activities because the facility is not accessible.
Yet the ADOC consistently houses prisoners with mobility impairments in facilities that are not accessible. With the exception of the Hamilton Aged and Infirmed Center, every facility contains architectural barriers for prisoners with mobility impairments. These failures turn everyday life for prisoners with disabilities into an obstacle course.
At Ventress Correctional Facility, a prisoner with limited mobility due to severe scoliosis needed to use a shower with a grab bar. He was told he could use the shower in the infirmary, two buildings away from where he was then housed. But the prisoner was later moved to the dormitory the farthest distance from the infirmary.
He was permitted to use the shower only late at night. This required him to make a painful 15-minute trek across the facility well past midnight to reach the shower. The prisoner asked to be housed near an appropriate shower, but was left in the distant dormitory for months. It was not until the SPLC and ADAP intervened on his behalf that he was moved to a location closer to an accessible shower.
At Kilby Correctional Facility a prisoner who is paralyzed on one side of his body and confined to a wheelchair is currently housed in B Dorm. The exit from B Dorm to the yard has steps, not a ramp. This dorm has no wheelchair-accessible bathroom facilities. The wheelchair-bound prisoner had no assistance when Kilby was recently evacuated for a fire. He also found no assistance when Kilby was evacuated for a gas leak. The prisoner struggled against the flow of evacuating prisoners to reach A Dorm, which is deeper within the prison but has a wheelchair-accessible exit.
At other ADOC facilities, prisoners with disabilities also find taking a shower or using the bathroom can be a needlessly difficult task. Restrooms throughout the system are not accessible. Toilets at several facilities are on raised platforms.
At Staton Correctional Facility, the only “accessible” shower is in the infirmary. The administrators at Staton claim that all persons with mobility impairments in the facility are housed in the infirmary to provide access to the shower. The shower in the infirmary is a raised metal shower stall with a plastic lawn chair in the middle and a hose for bathing. A prisoner must climb up a high step to enter. It is extremely difficult – if not physically impossible – for a prisoner who cannot walk or has limited mobility to independently enter this shower and use it. Moreover, there are several people with mobility impairments housed in other dormitories that do not have any form of accommodation for people with disabilities.
At Kilby’s A Dorm (the dormitory where prisoners with mobility and vision impairments are concentrated), the shower has an unstable chair. Several prisoners have reported falling while trying to get in and out of the shower chair.
Also at Kilby, there are currently nine wheelchair-bound prisoners in A Dorm. In recent years, there have been as many as 17 wheelchair users in A Dorm. The beds are so close that some of the wheelchairs cannot maneuver between the beds. The sole toilet accessible to these prisoners was not functioning for several months recently.
At the Kilby infirmary, there are a number of individual cells where the sink sits directly above the toilet, in the corner of the cell. A blind and wheelchair-bound prisoner was moved into one of these cells for several months. Because of his disability and the configuration of the toilet and sink, he had no access to the sink and had great difficulty getting to the toilet.
While ADOC need not ensure that all its facilities are accessible to persons with mobility impairments, it is impermissible to house those prisoners in locations that are not accessible. During the joint SPLC and ADAP inspections, wardens indicated that individuals were not housed in dormitories that were not accessible. These assertions were repeatedly contradicted by the presence of prisoners with disabilities in such dormitories and confirmation that they did indeed live there. Also, access to the outside in many facilities involves going down stairs.
Prisoners with disabilities improperly segregated
The ADOC has a long history of segregating prisoners with disabilities. This practice contradicts Title II of the Americans with Disabilities Act and its implementing regulations, which specifically require the ADOC to “administer services, programs, and activities in the most integrated setting appropriate to the needs of [prisoners] with disabilities.”
At least two blind prisoners were recently housed at Kilby Correctional Facility in A Dorm. This dorm is for persons with a Level 4 security classification, generally violent offenders. Neither prisoner had a history or conviction that warranted being housed in a Level 4 dorm. The justification for housing the prisoners in this dorm was “that’s where we put the blind people.” The same dorm also houses numerous people in wheelchairs, including those whose recommended security level is less than Level 4.
These prisoners are excluded from programming because the dormitory is part of the reception center, not a dormitory for those housed at Kilby. Also, it is often on lockdown because there is a high degree of violence, as is common in high-security, understaffed dormitories. Placing people in A Dorm because they are blind or wheelchair-bound is discriminatory and dangerous. Also, Title II’s implementing regulations specifically prohibit placing prisoners with “disabilities in inappropriate security classifications because no accessible cells or beds are available.”
Some facilities have the problematic policy of housing all persons with mobility impairments in infirmaries. Confining these prisoners to the infirmary deprives them of benefits, programs and services available to other prisoners. At Staton Correctional Facility, for example, mobility-impaired prisoners are housed in the infirmary. But the infirmary yard is extremely small and lacks the recreation equipment found in the regular yard used by the other prisoners.
No clear transition plan
These failures should not be surprising given the sparse evidence of planning by the ADOC to protect prisoners with disabilities from discrimination. The Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973 require the ADOC to develop a transition plan to ensure all programs, services and activities offered at its facilities are accessible to and usable by prisoners with disabilities.12 By no later than July 26, 1992, the ADOC should have developed a transition plan. But nearly 22 years after the deadline, it has not implemented a transition plan, and does not appear to have even developed such a plan.
If the ADOC indeed chose to make the structural changes necessary to comply with Title II of the Americans with Disabilities Act, such changes should have been completed by Jan. 26, 1995.13 Yet, the ADOC continues to operate inaccessible facilities and programs nearly 22 years after federal law mandated it make its programs accessible.
Even worse, few prisoners have the opportunity to voice complaints that could remedy violations of the Americans with Disabilities Act. Each ADOC facility should have at least one Americans with Disabilities Act coordinator to investigate a prisoner complaint of an ADA violation.14 Based on the investigation by the SPLC and ADAP, the Hamilton Aged and Infirmed Center appears to be the only facility with a coordinator and grievance procedure.