Profits vs. Prisoners: How the largest U.S. prison health care provider puts lives in danger
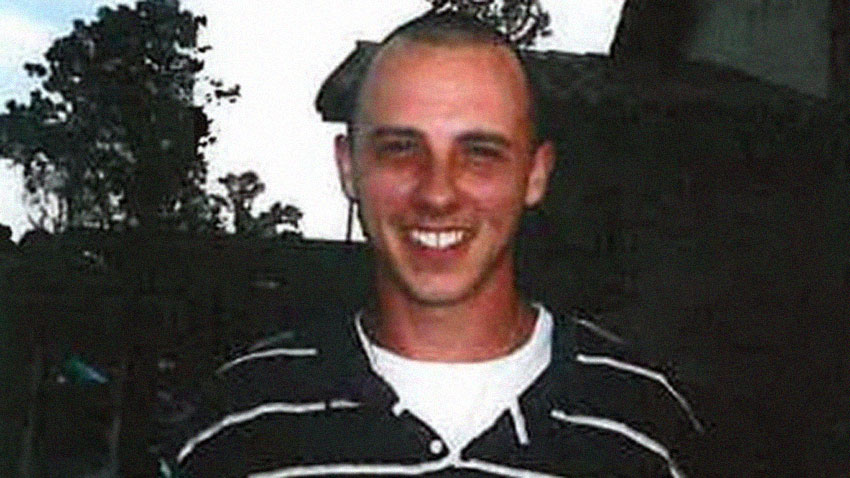
Kelly Green was off the medication he needed for his schizophrenia and was talking about killing himself. Alarmed by the homeless man’s erratic behavior on a cold Oregon night in February 2013, a convenience store clerk called the police.
When the Eugene police arrived, they arrested Green, 28, on an outstanding warrant related to a misdemeanor incident two months earlier.
At the Lane County Jail, Green cursed and talked to inanimate objects. A booking deputy wrote in her notes: “May be bipolar/schizophrenic. No meds … talks to himself … not making sense.” Although the prison health care giant Corizon Health Inc. had a contract to provide health screening and medical care at the jail, no one from the on-site Corizon staff made any effort to see Green or talk to him.
Green was placed in a cell by himself. He wasn’t provided with any psychiatric treatment.
The next morning, he snapped. During his arraignment inside a courtroom at the jail, a judge told him he would be detained for a couple of days. Green suddenly sprinted 10 feet toward a partition of concrete blocks, his head lowered. As skull met concrete, it sounded like “throwing a watermelon at the wall,” one observer later remarked.
What happened next illustrates much about what a growing chorus of critics across the country contends is fundamentally wrong with a privatized prison health care system that, at its core, exists to generate profits for investors. States and municipalities typically pay companies like Corizon a flat fee based on the number of prisoners for whom they provide care. The cold, hard reality is that every dime saved on prisoner care is a dime added to the company’s bottom line.
And when companies face financial difficulties – and it appears that Corizon does – their employees may face more pressure to cut costs by delaying or denying medical care to prisoners, as several former Corizon employees have alleged in court documents.
Though he suffered a catastrophic injury, later determined to be a “burst fracture” of the C-4 vertebra in his neck, Corizon employees chose not to send Green immediately to a hospital. Instead, court records show, they suggested that he be dropped off at the hospital after he was released from jail. In the meantime, he was humiliated and taunted by jail staffers as his condition grew progressively worse.
“If he had gone to the hospital before being released, Corizon would have had to pay the hospital bill,” said Elden Rosenthal, a Portland lawyer who represented Green’s family in a lawsuit against Corizon. “They had this system. There was something called a ‘courtesy drop.’ The physician’s assistant was thinking, ‘We’ll release this guy and then have the Lane County officers take him to the hospital.’”
It was almost seven hours before Green was transported to the hospital. By then, it was too late. He lost the use of his arms and legs, and was placed on a ventilator. He died from complications six months later. A medical expert for Green’s family said he would have been saved with timely intervention.
The life-and-death decisions made by Corizon staffers that day are the same kinds being made by the company’s employees in state prisons and local jails across America – decisions that inevitably weigh a patient’s medical needs against the cost to the company.
The Green case, like many others, raises the question of whether Corizon and its competitors place profits over the health and safety of prisoners who have no ability to choose their medical provider – and whether corrections officials should allow them to do so. The question is particularly important as the country begins to reform a criminal justice system that, with the world’s largest prisoner population, is viewed as a revenue stream by a collection of largely privately held corporations that exploit the privatization model for profit.
Corizon, owned and partly managed by a private equity firm in Chicago, was formed in a 2011 merger of two prison health care companies. Today, as the country’s largest for-profit prison health care provider, it’s responsible for the care of approximately 345,000 prisoners – about 15 percent of the U.S. prisoner population – at 534 correctional facilities in 27 states.
By all appearances, Corizon is under financial stress as it faces increasing scrutiny about its practices by prison officials, journalists and the courts. Hundreds of lawsuits are pending, many filed by inmates themselves, court records show.
In a September 2014 series of articles, The Palm Beach Post found that the company provided “deficient care” to Florida prisoners and reported that the number of deaths in the state’s prisons had reached a 10-year high. The company’s performance also has been criticized in government and court reports in Idaho, New York, Kentucky and Pennsylvania between 2012 and 2014.
At the time of The Palm Beach Post report, the company had annual revenues of $1.4 billion. About 14 months later, and after being fined $70,000 by the state for failing to meet contractual standards, Corizon walked away from its $1.1 billion, five-year contract with the Florida Department of Corrections. The move followed a decision by the credit rating service Moody’s to downgrade $360 million in Corizon debt securities, citing uncertainty about the Florida contract – the company’s largest – and other concerns about the company’s prospects.
In addition, in 2015, the company lost a contract with New York City, where it had provided health care for 11,000 prisoners at Rikers Island. Officials were concerned about 16 deaths there since 2009, according to The Associated Press.
Since 2012, Corizon also saw contracts terminated in Tennessee, Pennsylvania, Maine, Maryland, Minnesota and New Mexico. And it lost or walked away from several local jail contracts during that time. In California last year, Corizon and Alameda County agreed to pay $8.3 million to settle a claim by the family of a man who died after being beaten and Tased by jail deputies. Corizon’s share was $4.3 million.
Now, in Alabama, where Corizon holds a five-year, $405 million contract to provide health care to 25,000 prisoners, the Southern Poverty Law Center (SPLC) is suing the Alabama Department of Corrections (ADOC), charging that it is “deliberately indifferent” to the medical needs of the men and women in the nation’s most overcrowded prison system, where the mortality rate is among the highest of any state prison system. (Elden Rosenthal, the lawyer in the Oregon case, is a board member of the SPLC, but he has not worked on the SPLC case and SPLC lawyers did not work on the Green case in Oregon.)
The SPLC is seeking class action status so that it can represent all state prisoners in Alabama. The suit will likely be tried in federal court in Montgomery next year.
One prisoner, who served as a runner in the medical ward for years at an Alabama prison, told the SPLC that he has seen firsthand a Corizon-employed doctor’s reluctance to send other prisoners to an offsite hospital. He spoke to the SPLC recently. “Corizon,” he said, “has totally destroyed the medical department for the Department of Corrections.”
Citing the SPLC lawsuit, Corizon declined to comment on specific aspects of this report. The company’s director of external affairs, Martha Harbin, wrote in an email that the company delivers “a much-needed service to state and local governments in enabling them to meet their Constitutional obligation to provide inmates with healthcare that meets or exceeds the community standard of care.” She added that none of the clinical staff’s compensation is based on the financial performance of individual contracts or the company itself.
As part of its lawsuit, the SPLC commissioned Dr. Michael Puisis, a doctor and expert with years of experience reviewing prison health care as a consultant, to conduct a review of more than 2,300 “episodes of care” in Alabama’s prisons, focusing on prisoners with serious medical conditions.
He wrote in his report that the medical charts “demonstrate a lack of timely hospitalization” and that at least two deaths could have been prevented had Corizon employees sent prisoners to a hospital. In both cases, Corizon’s internal investigations found nothing the company could do to improve.
Puisis’ findings echo a core concern of critics who question the for-profit model of prison health care: whether the company purposely denies hospitalization to prisoners who need it. The Kelly Green case in Oregon raises the same question.
In Georgia, Corizon fired three employees, a doctor and two nurses, who raised concerns about hospitalization delays. The three all sued Corizon, claiming wrongful termination. None would comment for this report, but court documents provide a timeline of an episode that led to their allegations.
On Feb. 6, 2014, Matt Loflin, 32, landed in the Chatham County Jail after he was picked up on drug charges. He passed out in his cell four days later, then again on Feb. 11.
Betty Riner, one of the nurses who would later be fired, started work a week later. Corizon staffers then examined Loflin – 10 days after he had last lost consciousness – and found his heart rate elevated at 125 beats per minute. It looked like heart failure.
Over the next month in jail, Loflin would lose consciousness three more times, according to court records. A chest X-ray on March 20 showed his heart enlarged and its rate elevated, again, at 121 beats per minute. Loflin began pleading to go to the hospital, telling his cellmate to call his mother and tell her he was afraid he was going to die, according to an ongoing lawsuit filed against Corizon by his mother, Belinda Maley.
Corizon’s onsite physician, Dr. Charles Pugh, saw Loflin four days later and made a quick determination: Loflin needed to go to the hospital. He contacted Corizon’s regional medical director, his direct superior, for permission. He was denied but was allowed to set up an appointment for Loflin with a cardiologist; the cardiologist sent back test results consistent with heart failure.
Meanwhile, Loflin deteriorated. He held his chest in pain. His mother visited and left alarmed after seeing her son “disoriented, pale and bloated.” Staffers told her they had “difficulty getting him up” for the visit.
For 10 days, Pugh, Riner and another nurse, Lynn Williams, pleaded with their Corizon bosses to send Loflin to the hospital and every morning they were denied, according to the complaint they filed in court. In its response, Corizon denies this. Finally, Pugh hatched a plan to save Loflin: He would send him back to the cardiologist, who could then have Loflin admitted to the hospital.
It worked, but it was too late. Loflin’s blood pressure plummeted in the ambulance on April 7, nearly two months after he had first passed out in his cell. He lost consciousness for a fifth and final time that day and later died.
For Pugh, Riner and Williams, trouble was just beginning. They met with the Chatham County sheriff the following August to discuss their concerns about patient safety. On the same day, Corizon launched an investigation into the trio’s actions. “I met with Dr. Pugh and Ms. Williams,” their supervisor wrote in an email to Corizon’s human resources manager on Sept. 2. “Got nowhere with them.”
Pugh, Riner and Williams were fired later that year. In a lawsuit that lists several concerns for patient care, the three claimed they were fired “in retaliation for reporting that Corizon … is denying gravely ill patients admission to hospitals.”
Court records show their lawsuit was dismissed by a federal judge on Jan. 30, 2015, at their own request. It appears they could have reached an out-of-court settlement with Corizon or that the case was mediated through private arbitration.
That same day, Dr. Pugh entered a declaration in the Green case in Oregon. He described constant pressure from his Corizon bosses to save money by limiting emergency room visits. “Once or twice a week, there were telephone conferences I was expected to attend with the Corizon regional medical director regarding who was in the hospital and what was going on with patients in the hospital,” he wrote. “There was a constant demand to monitor all hospitalizations, to avoid hospitalizations, to request prompt hospital discharges and minimize hospital stays.”
Corizon, in fact, touted this monitoring to prospective clients. In a 2014proposal to the Missouri Department of Corrections, Corizon wrote of “decreased emergency room visits” and “quicker, more effective care during a true emergency.” The company provided charts showing examples of actual and target inpatient days, organized by regions of the country.
With the tracking, and constant pressure on doctors like Pugh, Corizon could maximize profits by discouraging hospital visits, according to the lawsuit filed by Loflin’s family in Georgia. The prices paid by states and municipalities for Corizon’s services were set by “average daily population” of jail and prison facilities, several of the company’s contracts show. That meant that payments to hospitals came out of the money Corizon received from the government.
“If I give you $100 to take a stranger out to lunch, and I tell you, ‘You can keep whatever you don’t spend on the stranger’s lunch,’ then where are we going to lunch?” said Will Claiborne, the lawyer who represents Loflin’s family and also represented the three fired Corizon employees. “Or in these inmates’ cases, will they be getting lunch at all?”
Pugh and Puisis both say that Corizon’s regional medical directors apply pressure when it comes to hospitalizations. They do so with full knowledge that, as Claiborne put it in his complaint on behalf of Loflin’s family, “any hospitalization had the potential to undermine Corizon’s profit margin.”
In his report for the SPLC in Alabama, Puisis describes how a Corizon regional medical director intervened to cut short a hospital stay for a patient at the Ventress Correctional Facility who had a massive infection affecting his entire right leg. After the Corizon’s medical director at the facility called the hospital three times asking for the patient’s release, “the regional medical director called and asked to have the patient sent back to prison,” Puisis wrote. “The hospitalist reluctantly returned the prisoner but documented that he thought the patient needed continued hospitalization.”
With the decisions to hospitalize or not hospitalize a prisoner made at the regional level of the company’s hierarchy, together with the corporate tracking of “inpatient days” by region, the same problem can arise at different ends of the country. Corizon has baked this “keep what you don’t spend” structure into its contracts around the country, with similar contracts in at least Missouri, Wyoming and New Mexico, an SPLC review shows.
The company is, after all, in business to make profits for investors. At the top of the chain of companies that controls Corizon is the private equity firm Beecken Petty O’Keefe and Co., a Chicago-based company that specializes in the sort of financial transactions – buyouts and corporate restructuring – that have made fortunes for the likes of 2012 Republican presidential nominee Mitt Romney.
In brochures aimed at its wealthy clientele, Beecken Petty plays up its role in directing the companies in its portfolios, like Corizon. The pitch is loaded with talk about “financial objectives” and “increasing equity value.” It boils down to this: The Chicago financiers say they help direct their companies’ activities.
The largest of Beecken Petty’s investment funds counts Corizon and four other companies in its portfolio, according to the equity firm’s website. The fund’s asset value sagged last year: It posted a value of $257.8 million in March 2016, compared to $398 million the previous year, according to financial disclosures.
Though it’s unclear whether Corizon’s performance contributed to that drop, it’s likely that forced retreats from major contracts didn’t help matters. The Moody’s report in October 2015 that downgraded the debt securities of Corizon’s holding company, Valitas Health Services, noted the company’s “high financial leverage” – its significant debt – in addition to risks associated with the “volatility of its contracts” and “margin compression due to competitive pricing pressure in renewed contracts.”
The company received one more bit of bad news after the Loflin case: Corizon would have to walk away from Chatham County, Georgia, where a new sheriff campaigned on providing better care to inmates.
The details of what happened to Kelly Green immediately after he ran headfirst into a wall in the Lane County Jail courtroom in Oregon on Feb. 12, 2013, are murky.
A Corizon physician’s assistant claims Green could move as she performed a neurological exam. Others dispute that, saying Green could not move and that he told the physician’s assistant he could not move. The county deputies at the scene recall someone asking the physician’s assistant whether Green should be taken to the hospital. No, she said, according to court filings, it’s not necessary.
She did, however, suggest dropping Green off at a hospital once the jail released him – a “courtesy drop.”
He was taken to the jail’s medical clinic 10 minutes after he injured himself, beginning several hours of dangerous and humiliating treatment at the hands of deputies, all captured on video.
Corizon staffers and the deputies offer conflicting accounts of who discussed hospitalization for Green and when. The Corizon regional medical director said he didn’t “recall hearing anything about Mr. Green while he was in jail,” according to a memorandum filed by the lawyer Rosenthal.
Meanwhile, Green lost control of his bowels – a classic sign of spinal cord injury. Unable to move, deputies laughed as they taunted him. He fell out of the wheelchair the jailers had been using to transport him.
It wasn’t until nearly 4 p.m. that day, more than five hours after he ran into the wall, that video confirms someone with Corizon saying Green needs to go to the hospital. “I was under the impression he was going to be released within an hour or two … we were going to have you guys do a drop,” the physician’s assistant says in the video. “He needs to go now.”
With his vital signs indicating severe shock, according to the court filing, Green had to wait another hour for paramedics to arrive.
Green went to the hospital at 5:30 p.m. By 7:46 p.m., he was in surgery.
Ultimately, it wouldn’t save him. Green left the hospital a quadriplegic, unable to move or use his arms or legs, and dependent on a ventilator to breathe. Complications from ventilator dependence led to his death six months later.
Rosenthal quotes an expert on spinal cord injuries in his court filing. The expert opinion: Had Kelly Green been promptly taken to the hospital, he would have lived. In July 2015, Corizon reached a financial settlement with Green’s family. The terms are confidential.
June 2011 – Two companies, Prison Health Services and Correctional Medical Services, merge to create Corizon Health Inc. The new company is owned by the private equity firm Beecken Petty O’Keefe and Company through a holding company, Valitas Health Services Inc. Corizon has more than 11,000 employees and $1.4 billion in annual revenue from contracts to provide health care at more than 400 correctional facilities nationwide.
March 2012 – A report commissioned by a federal judge calls Corizon’s care for Idaho prisoners “cruel and unusual.” The state fines the company $200,000 for missing contract benchmarks.
June 2012 – Corizon loses its contract with Maine’s prison system after a state audit accuses the company of failing to meet the basic health care needs of inmates on time.
October 2013 – Minnesota cuts 15-year ties with Corizon, awarding a state contract to another company despite Corizon having the lowest bid. A Star Tribune investigation found nine inmate deaths attributable to Corizon’s poor care since 2000.
June 2014 – The SPLC sues the Alabama Department of Corrections, alleging that it is “deliberately indifferent” to the medical needs of prisoners and has failed to provide constitutionally adequate mental health care. Corizon, the medical provider, is not named as a defendant.
January 2015 – Tennessee dumps Corizon for a competitor, Centurion, even though Corizon had submitted a lower bid.
February 2015 – Alameda County, Calif., and Corizon agree to pay $8.3 million to the family of an inmate who died after being beaten and Tased by jail staff. Corizon’s share is $4.3 million. The settlement is the largest of its kind in California history.
June 2015 – A New York City report finds that Corizon failed to perform adequate background checks on employees, resulting in the hiring of eight staffers with criminal records. Mayor Bill de Blasio announces his administration will not renew the company’s contract to provide health care at Riker’s Island.
August 2015 – Corizon reaches a confidential financial settlement with the family of Kelly Green in Oregon. Green died six months after a spinal injury that was self-inflicted while incarcerated in the local jail. His family claimed in court that the company’s delay in taking him to the hospital contributed to his death.
October 2015 – Moody’s downgrades the credit rating of Corizon’s parent company, Valitas Health Services. Analysts cite the company’s significant debt and uncertainty about its Florida contract.
November 2015 – Corizon walks away from its five-year, $1.1 billion contract with the state of Florida after enduring months of media scrutiny and paying a $70,000 fine for failing to meet care standards.
May 2016 – New Mexico picks a Corizon competitor to take over health care services in its prisons. Corizon had serviced the state’s prisons since 2007.
June 2016 – Corizon leaves the Chatham County jail in Georgia when a new sheriff takes office after having staked his campaign on improving prisoner health care.